Retraining Your Body’s Nervous System to Overcome Chronic Pelvic Pain
Our Body’s Nervous System is Wired like a Home Security System.
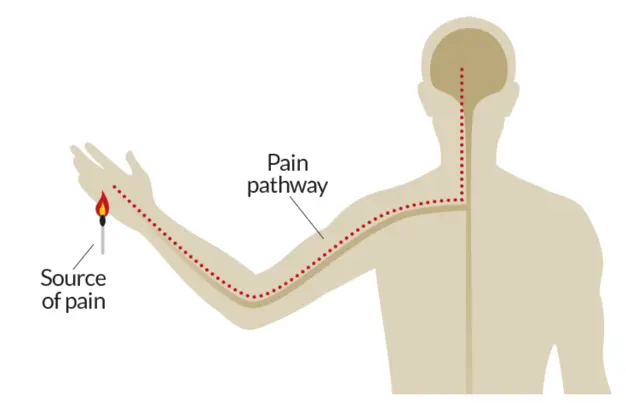
Our body’s nervous system includes the brain, spinal cord and all the peripheral nerves that branch out to the rest of your body including the skin on your fingers, muscles in your feet and tissues in your organs. The cells in the nervous system conduct messages between these tissues and your brain or spinal cord. These messages include ones where your brain is telling your arm to move, or the other way around where the nerves in your hand are telling your brain that you’re touching something hot.
Pain is a normal human experience. It is a protective mechanism that we develop from birth that is necessary for our survival. Without pain, humans would not know to let go if holding something too hot or when it’s time to clean out an open wound.
Our body’s nervous system is like a home security system.
- Similar to the wiring of a house’s alarm system, there is electricity coursing through the nerves in our body at all times.
- Our nerves fire a message to our brains when they reach a certain stimulus’ threshold, similar to when smoke reaches the sensor of a fire alarm
Simulti can be categorized as
- mechanical (I.e. straining a muscle)
- thermal (I.e. touching a hot pan) or
- chemical (I.e. eating a jalapeno pepper that’s too spicy).
When your brain receives this message from your nerves, it produces the feeling of pain in order for you to take action to mitigate the stressor.
Fight/Flight or Rest/Digest?
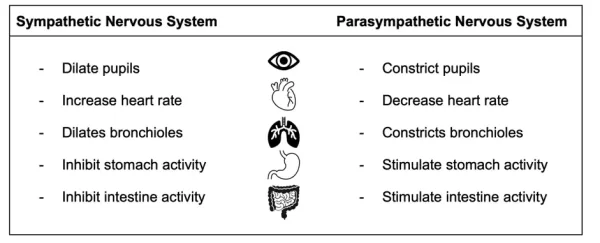
The nervous system has two different states. The first is the sympathetic nervous system, which is your fight or flight state that switches on when faced with a threat.
The second state is the parasympathetic nervous system, which is your rest and digest state. Your body should remain in this state so long as you are not faced with any threat.
The body responds differently when your nervous system switches between each of these states. Below is a chart describing how various organs in the body are affected when your sympathetic or parasympathetic nervous system takes over.
Acute vs Chronic Pelvic Pain
When your body is exposed to an injury, your body’s alarm system will activate and your nerves will become slightly more sensitive. As your injury begins to heal, your nerves will slowly return back to its resting level of sensitivity. This is what we characterize as acute pain.
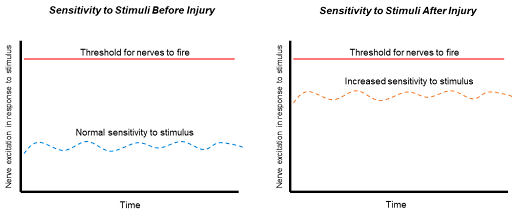
Once the physical injury begins to heal, the body’s alarm system will return to its resting state and your body will not feel pain as frequently. In patients with chronic pain, your body’s alarm system may remain heightened even if your injury is healed.
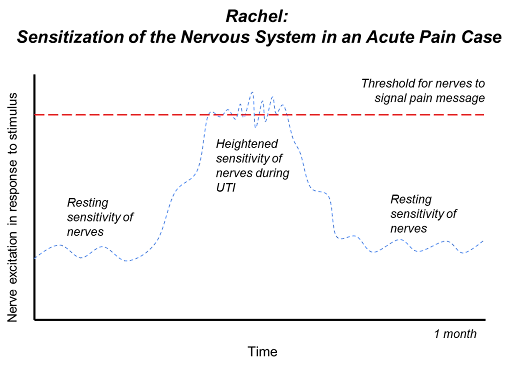
Rachel recently starts to feel the need to urinate more frequently and feels pain when she goes to pee. She visits her family doctor, is diagnosed with a urinary tract infection (UTI) and is placed on antibiotics.
Every time she urinates, washes in the shower or sits and feels her underwear rubbing against her tissues, she feels pain. Her tissues have developed an increased sensitivity to the same everyday stimuli that would not have triggered her pain before the UTI.
As she finishes up her antibiotics, her UTI symptoms resolve along with her pain. This is a scenario where the patient is experiencing acute pain. Her nervous system is more sensitive and her brain produces more pain sensations over a short period of time. Once her tissues begin to heal, the sensitivity decreases back to her baseline. Rachel only has this one UTI over the next few years.
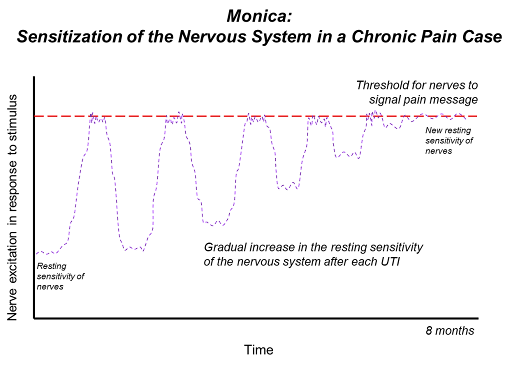
Monica experiences the same symptoms and is also diagnosed with a UTI. During this time, she also experiences pain with urination and when she feels her underwear rubbing against the irritated tissue.
Her nerves also increase in sensitivity for a short period of time. She finishes up her antibiotics and the pain leaves. Then, over the next 8 months, she proceeds to have 4 more UTI’s.
Unlike the first UTI, each time her nervous system is heightened with the subsequent UTI’s, it does not quite go down to its baseline. After 8 months, the new resting sensitivity of Monica’s nervous system sits at a much higher level than before.
This new resting state sits right at her pain message firing threshold causing Monica to feel vaginal irritation with stimuli like rubbing against her underwear which she may not have felt pain with before.
Hurt vs Harm
To understand the complexity of chronic pain, it is important to consider the difference between feeling hurt versus actual harm in Monica’s case. Prior to her first UTI, Monica would never feel pain when sitting on a bus and feeling her underwear rub against her vaginal tissue.
We also know that this stimulus was not causing any physical harm to her prior to her first UTI. Now, after her 5th UTI, her nervous system is so sensitive and on guard that even the sensation of her underwear rubbing against her skin feels like a threat to the body.
However, we still know that this sensation from her underwear is not causing her any physical harm. This is where we need to downtrain the nervous system to properly differentiate the feeling of hurt versus actual harm again.
We want a home alarm system to go off when a thief is actually trying to break into the house, not when it’s just a neighbour coming home and parking into their own garage!
Understanding Psychosocial Influences on Pain
It is also important to acknowledge that there is a psychosocial component to the pain experience. Take the example of a UTI under two different scenarios:
- A Hectic week before going on vacation
Imagine you have travel plans to Cuba next week and all week you’ve been stressing to hand things off with work, trying to finish packing and your 4 year old toddler gets pink eye from school. Two days before the trip, you start to feel an irritation when you pee and have to pee a lot more frequently. You rush to get a last minute appointment with your doctor who tells you you have a UTI and have to be on antibiotics for the next week.
2. A slow week after the Holidays
Imagine a second scenario where it’s the beginning of the year and all your social meet-ups over the holidays are done with. You’re working from home and there isn’t much in way of deadlines for you to meet. Your parents are in town and they have been able to help out a lot with the little one.
You then start to feel symptoms and your doctor diagnoses you with a UTI. Your experience with recovering from the UTI in the second scenario is going to be a lot less stressful and aggravating than the first.
This example helps us understand the effects of external factors on one’s pain experience. In both scenarios, the painful stimulus is the same. However, the surrounding factors and environment plays a large role on how the experience of having a UTI changes. This can be relevant to any pain experience and any life stressor that may add to your pain experience.
Retraining your Body’s Nervous System
It’s often referred to as “downtraining the nervous system”, but this is where a pelvic floor physiotherapist can help your body relearn how to differentiate the sensations of hurt vs harm.
- Employing strategies to improve movement of the pelvic floor and hip muscles
- Desensitizing problematic areas with manual therapy
- Developing body awareness and pelvic floor muscle control
- Developing breathing techniques and cues to initiate pelvic floor muscle control
A combination of these techniques selected specifically for each client can help re-teach the nervous system what non-harmful stimuli is.
Ultimately, our goal as pelvic floor physiotherapists is to help you retrain your nervous system so you can progress towards pain-free activities in your daily life.